If you’re experiencing intense sadness, emotional numbness, guilt, or pervasive prolonged grief months after the death of a loved one, you may wonder:
“How long will these feelings continue?” or “Will grief stay this painful forever?” or “Can grief be permanent?”
Is prolonged grief the same as complicated grief?
If you have heard of prolonged grief disorder or complicated grief, you may ask:
What's considered prolonged grief?
Is prolonged grief the same as complicated grief?
At what point should one seek professional grief support?
Grieving is a universal experience. Losing a loved one is one of the most challenging and stressful experiences we can have as humans.
Sometimes it may feel as if our grief will last forever.
Most grievers will, in time, adjust to a loss and resume meaningful activities and relationships.
The death of a loved one is one of the most difficult and stressful life experiences.
However, a small proportion of bereaved individuals experience intense emotional pain or emotional numbing that prevents socializing, working, or otherwise engaging in life for more than a year following a loss.
For these individuals, grief can become incapacitating.
The American Psychiatric Association (APA)’s description of prolonged grief disorder (PGD) may match their experience.
In March 2022 the APA released the text revision of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) which included the definition and diagnosis of prolonged grief disorder (PGD).
Most grievers will, in time, adjust to a loss and resume meaningful activities and relationships.
Below we’ll find out more about prolonged grief, also known as complicated grief.
We’ll outline the official prolonged grief disorder symptoms to better understand the meaning of prolonged grief and how to get help and treatment if needed.
What are the symptoms of prolonged grief disorder?
People suffering from prolonged grief disorder experience intense emotional pain, including sadness, guilt, or anger, or emotional numbness.
They also may have difficulty accepting the death of their loved one.
If you’re concerned you or someone you know might be suffering from PGD, here signs and symptoms to note.
Some bereaved individuals experience intense emotional pain that prevents socializing, working, or otherwise engaging in life more than a year following a loss.
The APA describes prolonged grief disorder as “intense yearning or longing for the deceased (often with intense sorrow and emotional pain), and preoccupation with thoughts or memories of the deceased (in children and adolescents, this preoccupation may focus on the circumstances of the death).”
According to the APA’s diagnostic criteria, to be considered prolonged grief disorder, the death must have occurred at least one year before the diagnosis of PGD for an adult, and at least six months before the diagnosis of PGD for a child or adolescent.
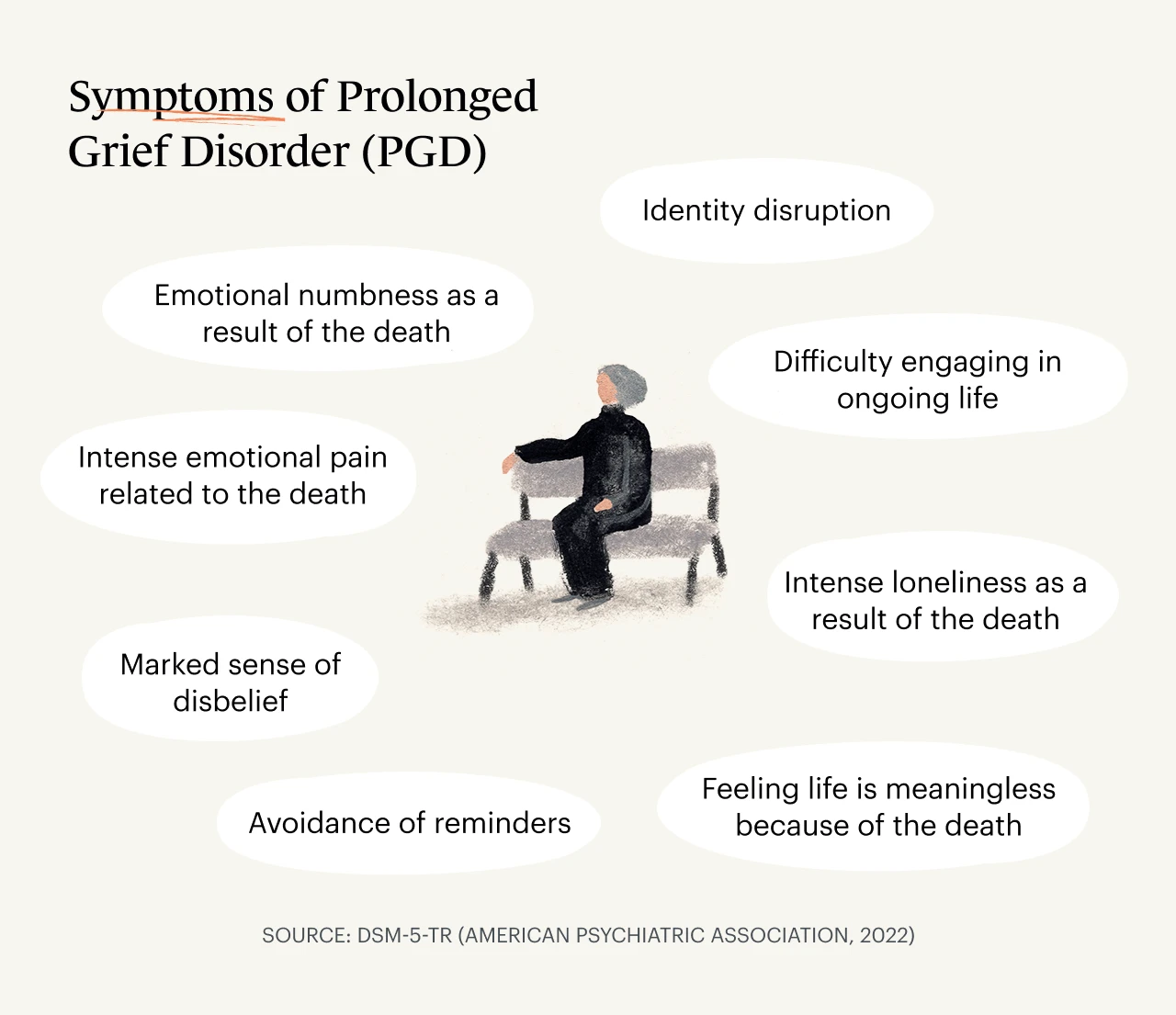
Prolonged grief disorder symptoms are described in the DSM-5-TR as
Persistent and pervasive yearning, longing, or preoccupation with the deceased
At least three of the following symptoms nearly every day for at least the past month:
Identity disruption
Marked sense of disbelief
Avoidance of reminders
Intense emotional pain related to the death
Difficulty engaging in ongoing life
Emotional numbness as a result of the death
Feeling life is meaningless because of the death
Intense loneliness as a result of the death
Clinically significant distress or impairment in personal, family, social, educational, occupational, or other important areas of functioning
Duration and severity of the bereavement reaction clearly exceed expected social, cultural, or religious norms for the individual’s culture and context
PGD is typically diagnosed following a structured clinical interview with a psychiatrist, psychologist, or other mental health professional.
How many people does PGD affect?
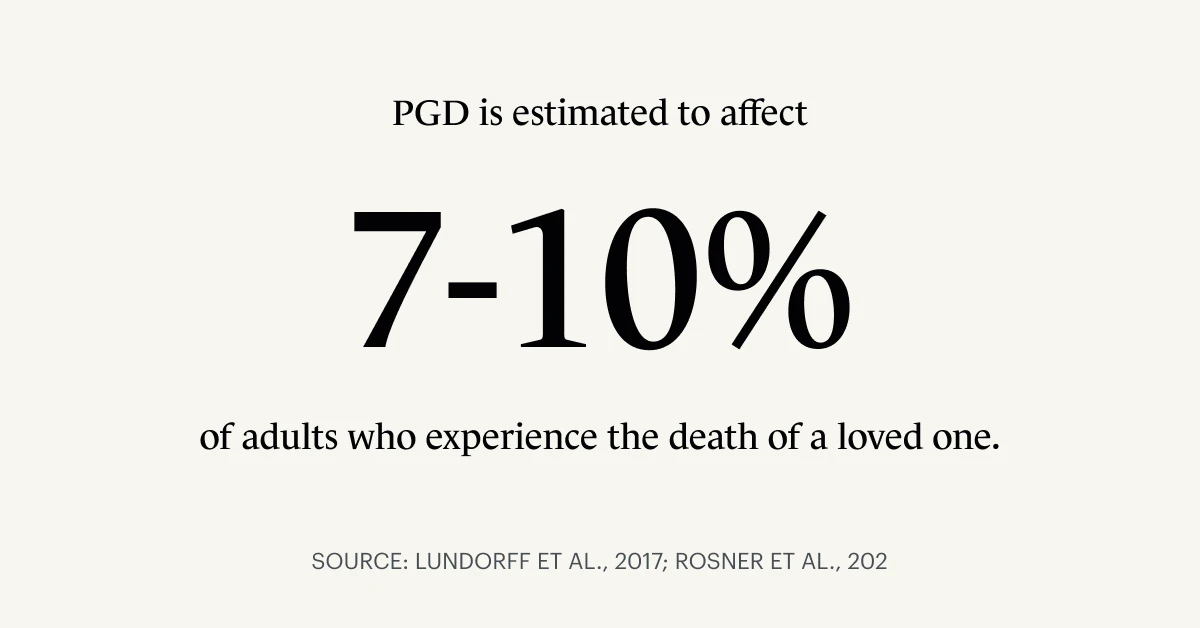
Prolonged grief disorder is estimated to affect 7-10% or more of adults who experience the death of a loved one according to a 2017 meta-analysis and a 2021 study of college students.
Data referred to in a 2021 article by Dr. Kristin L. Szuhany, Ph.D., suggest that PGD is more prevalent in those who have a history of major depressive disorder or bipolar disorder, those who acted as the primary caregiver for the deceased, or those whose loved one died unexpectedly or by tragic means, such as homicide, suicide, or accident.
Is prolonged grief the same as complicated grief?
Research groups, including those led by Dr. M. Katherine Shear, M.D., and Dr. Holly G. Prigerson, Ph.D., have studied prolonged grief since the 1990s.
Initially, researchers used the term complicated grief, but it has since been replaced by prolonged grief.
And is persistent complex bereavement disorder (PCBD) the same as prolonged grief disorder (PGD)?
In 2013 the DSM-5 included persistent complex bereavement disorder (PCBD) in the appendix as a disorder requiring further study.
Research published in 2016 using data derived from the Yale Bereavement Study, a longitudinal community-based study of bereaved individuals provided evidence that prolonged grief disorder and persistent complex bereavement disorder reflect the same condition.
How has the addition of prolonged grief disorder to the DSM been received?
Supporters of prolonged grief disorder’s inclusion in the DSM believe defining a separate diagnosis for PGD will advance prevention and early intervention efforts to identify those most at risk of suffering prolonged grief.
In addition, supporters argue it could promote funding for the development of effective treatments for prolonged grief and create opportunities for more discourse and connection for those who experience PGD and complicated grief.
Another benefit of DSM classification is that medical and mental health professionals can now bill health insurance providers so that patients with insurance may be able to get their providers to cover the cost of treatment for PGD.
Hopefully coverage by insurance will contribute to expanded access to care.
The DSM classification of prolonged grief disorder means patients with health insurance may be able to get their treatment for PGD covered by insurance.
On the other hand, critics opposed to the addition of PGD in the DSM-5-TR argue that the spectrum of grieving should not be medicalized. They believe labeling grief-related feelings and behaviors as “disordered” may add to stigma.
Some critics warn about the risks of over-diagnosing and overprescribing psychotropic medication for the bereaved.
Researchers and advocates caution that centering a “problem” within an individual ignores societal shortcomings in how we support grievers, especially those who experience stigmatized losses, including death from suicide, homicide, or substance-related causes.
A mix of critics and supporters question the criteria of “12 months since loss” for adults.
Some critics argue that 12 months is premature for resolving profound grief, while others reason that earlier diagnosis and intervention may provide earlier help and support for those suffering.
Treatments for prolonged grief disorder
If you’re concerned you may be suffering from prolonged grief disorder, reach out to a primary care doctor, clinical psychologist, psychiatrist, and/or a therapist or counselor specializing in grief.
Be sure to let them know how you are feeling.
If they do not have specific expertise and training in assessing and treating prolonged grief disorder, ask if they might be able to refer you to a clinician who does.
Here are some specific types of treatment that can be helpful for those suffering grief or prolonged grief disorder.
Prolonged grief disorder therapy (PGDT)
The prevailing evidence-based treatment for PGD is prolonged grief disorder therapy (PGDT), formerly known as complicated grief therapy (CGT), a 16-session, one-on-one talk therapy developed by researchers at Columbia University led by psychiatrist Dr. Shear.
Sessions are structured, and move from agenda setting to loss-focused content, restoration-focused dialogue, and planning for the next week.
Described in Dr. Szuhany’s 2021 article, the approach in PGDT emphasizes seven themes, which aim to “help patients understand and accept grief, managing emotional pain and monitoring symptoms, thinking about the future, reconnecting with others, telling the story of the death, learning to live with reminders, and connecting with memories.”
This course of therapy includes imaginal and situational exposure to address avoidance of reminders and practice managing difficult emotions.
Clinical studies including this one from 2016 have found that PGDT is effective at improving mood and functioning. Another 2013 study among older adults found PGDT is also effectively applied in a group therapy setting.
Because PGDT is a specialized treatment, not yet widely available to all people who may be suffering prolonged or complicated grief, there are other options to consider to ensure individuals with prolonged grief disorder get the support they need.
Grief counseling or grief therapy
If you’re experiencing grief of any kind—including prolonged or complicated grief—you can also seek therapy or grief counseling for support and healing.
Participating in one-on-one therapy sessions can help you work through your emotions with a trained mental health professional to feel better equipped to process the feelings and re-engage with meaningful activities and relationships.
The Monarch Directory by SimplePractice contains licensed counselors and therapists specializing in grief.
You can view their individual profiles to determine whether they accept your health insurance.

Many of these experienced grief counselors offer online booking, in-person sessions, telehealth video appointments, and free 15-minute initial consultations to help you determine if they’re the right fit for your needs.
Whether or not you have health insurance—if you want to see a therapist or counselor—there are also free, low-cost, and affordable therapy options.
3 types of counseling for grief
You may be wondering which types of therapy have demonstrated effectiveness in supporting and healing those who are grieving.
Here are a few key therapeutic approaches with some evidence-based results.
1. Cognitive behavioral therapy (CBT)
Cognitive behavioral therapy helps people identify unhelpful thoughts and thought patterns and behaviors and develop more adaptive thoughts and responses.
A 2021 study found that “prolonged grief disorder and its symptoms in bereaved children and adolescents can be effectively treated by CBT interventions.”
An active study aims to better understand the efficacy of cognitive behavioral therapy among older adults suffering from prolonged grief.
View therapists near you who specialize in CBT.
2. Acceptance and commitment therapy (ACT)
Acceptance and commitment therapy helps people accept, rather than avoid, emotions such as grief following the death of a loved one, become more mindful of negative thoughts, develop clarity about personal values, and commit to behavior that serves one's values.
According to Los Angeles-based Monarch clinical psychologist Dr. Nikki Rubin, PsyD, who specializes in acceptance and commitment therapy, ACT uses behavioral science in concert with mindfulness to “help build us the lives we want even in the presence of pain.”
A 2017 study found that ACT reduced anxiety and increased bereaved patients’ life expectancy.
View therapists near you who specialize in ACT.
3. Mindfulness-based cognitive therapy (MBCT)
Mindfulness-based cognitive therapy (MBCT) and mindfulness practices can help people non-judgmentally observe feelings of grief and their effects.
A 2021 study noted that “MBCT improves the well‐being of the bereaved by enhancing cognitive performance.”
Another small 2013 study of bereaved participants in their seventies concluded “MBCT appears to reduce depressive symptoms in this sample of elderly bereaved people, but further studies of the effects of MBCT in this population are needed for firm conclusions.”
View therapists near you who specialize in MBCT.

Prolonged grief disorder therapy (PGDT)
Also known as complicated grief treatment (CGT), PGDT is mentioned above, and more information is included below.
4. Group therapy
In-person and online support groups and group therapy can be excellent options for those grieving or experiencing prolonged grief.
In group sessions, you’ll connect with others who have lost someone close to them.
Many grief support groups are free.
After losing her husband Dave Goldberg, Facebook COO Sheryl Sandberg created Option B, which has a free community sharing content on grief, as well as a free private Facebook support group, which anyone can join to connect with others who are bereaved and grieving to share stories and support each other.
Other grief support groups include Gilda’s Club, for those impacted by cancer, and Compassionate Friends, a support group for those who have lost children.
How to get help with prolonged grief
If you are seeking evaluation or care for grief that feels debilitating, it’s important to connect with a medical professional or mental health professional with expertise in grief, and optimally someone who has training in the assessment and treatment of prolonged grief.
The Center for Prolonged Grief at Columbia has a directory of clinicians trained in the Prolonged Grief Disorder Therapy (PGDT) treatment, discussed earlier in this article.
The Monarch directory contains thousands of licensed counselors and therapists specializing in grief.
Many offer online booking, in-person sessions, telehealth video appointments, and free 15-minute initial consultations to help you determine if they’re the right fit for your needs.

Is grief therapy appropriate for those who do not meet the criteria for PGD?
Many people who do not develop prolonged grief disorder or complicated grief will still benefit from grief support, whether through individual therapy, a support group, or reading non-fiction or grief memoir.
The Monarch directory includes thousands of counselors and therapists who specialize in helping clients with grief.
Many will find that grieving never ends. Over time, however, we adapt and find meaning and satisfaction in other relationships and pursuits.
For those whose years following loss continue to be dominated by intense emotional pain and difficulty engaging with life, a diagnosis of prolonged grief disorder may provide access to tailored therapeutic treatment that creates a path toward meaningful healing.
Consider reaching out for help and support.
Concerned you may be depressed?
Depression is distinctive from grief. However people can experience new or worsening depression following a significant loss.
Take our online depression assessment to determine whether you may be experiencing symptoms of depression.
We recommend you speak with someone—a trusted family member, friend, doctor, or therapist—about how you're feeling.
Here are counselors who specialize in helping clients with depression. You may wish to contact for a consultation or session.
Additional resources if you’re experiencing suicidal thoughts or depression
The National Suicide Prevention Hotline is toll-free, 24/7 support. The phone number is 1-800-273-8255. You can also call or text them at 988.
The National Alliance on Mental Illness provides information and support for those who experience mental illness, and their families and caretakers.
The Suicide Awareness Voices of Education (SAVE) foundation provides resources for those who have survived a loss by suicide.
READ NEXT: What's the Difference Between Grief and Loss?
Need to find a grief therapist who may be able to help you with prolonged grief or complicated grief? Check out the Monarch Directory by SimplePractice to view grief counselors near you with availability and online booking.
References
American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (Dsm-5-Tr(tm)). American Psychiatric Association Publishing.
Lundorff, M., Holmgren, H., Zachariae, R., Farver-Vestergaard, I., & O’Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders, 212, 138–149.https://doi.org/10.1016/j.jad.2017.01.030
Maciejewski, P. K., Maercker, A., Boelen, P. A., & Prigerson, H. G. (2016). “Prolonged grief disorder” and “persistent complex bereavement disorder”, but not “complicated grief”, are the same diagnostic entity: an analysis of data from the Yale Bereavement Study. World Psychiatry, 15(3), 266–275. https://doi.org/10.1002/wps.20348
Rosner, R., Comtesse, H., Vogel, A., & Doering, B. K. (2021). Prevalence of prolonged grief disorder. Journal of Affective Disorders, 287, 301–307.https://doi.org/10.1016/j.jad.2021.03.058
Shear, K., Frank, E., Houck, P. R., & Reynolds, C. F. (2005). Treatment of Complicated Grief. JAMA, 293(21), 2601. https://doi.org/10.1001/jama.293.21.2601
Shear, M. K., Reynolds, C. F., Simon, N. M., Zisook, S., Wang, Y., Mauro, C., Duan, N., Lebowitz, B., & Skritskaya, N. (2016). Optimizing Treatment of Complicated Grief. JAMA Psychiatry, 73(7), 685. https://doi.org/10.1001/jamapsychiatry.2016.0892
Supiano, K. P., & Luptak, M. (2013). Complicated Grief in Older Adults: A Randomized Controlled Trial of Complicated Grief Group Therapy. The Gerontologist, 54(5), 840–856. https://doi.org/10.1093/geront/gnt076
Szuhany, K. L., Malgaroli, M., Miron, C. D., & Simon, N. M. (2021). Prolonged Grief Disorder: Course, Diagnosis, Assessment, and Treatment. FOCUS, 19(2), 161–172. https://doi.org/10.1176/appi.focus.20200052




