Mental health stigmas are negative judgments aimed at people with mental illness or anyone who is seeking counseling, therapy, or support for mental health concerns.
Stigmas around mental health come in many forms and can be downright dangerous.
For example, mental health stigma can cause shame and make it seem frightening or embarrassing for people to discuss common and treatable mental health disorders, such as anxiety, depression, substance abuse, ADHD, trauma, and PTSD.
Stigmas around mental health come in many forms and can be downright dangerous.
Stigma can discourage us from speaking with a therapist or counselor or talking openly about our mental health needs with family and friends.
What’s more, there are specific groups of people who have historically faced increased stigmatization around seeking mental health support and therapy, including American men, Asian Americans, and Black Americans.

First, what’s the definition of stigma?
Stigma is defined as a “mark of disgrace associated with a particular circumstance, quality, or person.”
As Julio Arboleda-Flórez, M.D., Ph.D., points out in a 2003 article, "Stigma, prejudice, and discrimination are closely related and tightly interwoven.”
And they’re all quite negative.
“Stigma, prejudice, and discrimination are closely related and tightly interwoven.”
Here’s how it works: According to the authors of this 2021 research, stigmatization causes individuals to be discredited, devalued, and shamed because of specific characteristics or attributes they possess.
Stigma typically leads to negative social experiences, such as isolation, rejection, marginalization, and discrimination, the authors of the research point out.
One of the most widely read sociologists in history, Erving Goffman, Ph.D., brought the term stigma into the mainstream during the 1950s and 1960s.
In his 1963 best-selling book Stigma: Notes on the Management of Spoiled Identity, Goffman defines stigma as a means of “spoiling” stigmatized individuals’ or groups of people’s identity, status, and reputation in society.
Stigma typically leads to negative social experiences, such as isolation, rejection, marginalization, and discrimination.
“By definition, of course, we believe the person with a stigma is not quite human,” Goffman writes. “On this assumption we exercise varieties of discrimination, through which we effectively, if often unthinkingly, reduce the individual’s life chances.”
3 main types of stigma
Goffman identified three main types of stigma:
Stigma associated with mental illness
Stigma associated with physical differences
Stigma attached to identification with a particular gender, race, ethnicity, religion, ideology, etc.

What are 4 kinds of stigma associated with mental health?
According to the American Psychological Association (APA), stigma, prejudice and discrimination against people with mental illness is still a sizable issue.
There are at least four types of mental health stigmas:
Self-stigma
Public stigma
Professional/work stigma
Institutional stigma.
Self-Stigma
Self-stigmas around mental health, as defined by the APA, are “the negative attitudes, including internalized shame, that people with mental illness have about their own condition.”
Self-stigmas are “the negative attitudes, including internalized shame, that people with mental illness have about their own condition.”
Public Stigma
Public mental health stigma, as described in a 2002 research paper, is “the reaction that the general population has to people with mental illness.”
The authors point out that—as a result of the stigma, stereotypes, and prejudices—people with mental disorders are often “robbed of the opportunities that define a quality life: good jobs, safe housing, and satisfactory health care.”
Public stigma is a very common form of mental health stigma. It can come from friends, family, and even the media we consume.
Public mental health stigma can cause us to isolate ourselves from loved ones who have expressed negative attitudes about our mental health disorder or challenges.
Public stigma is a very common form of mental health stigma. It can come from friends, family, and even the media we consume.
A 2013 systemic review of research on public stigma found that stigmatizing beliefs most often led to discrimination.
Many study respondents reported avoiding people with mental health disorders because they believed them to be dangerous and unstable.
Work/Professional Stigma
Professional and work stigma around mental health can persist even in the most progressive workplaces, according to Don Mordecai, M.D., who wrote an article on this topic for Kaiser Permanente.
Employees keep their conditions secret, because they “may be afraid that being open about them will hurt their reputation, compromise work relationships, or even jeopardize their jobs.”
Mordecai points out many employees keep their conditions secret, because they “may be afraid that being open about them will hurt their reputation, compromise work relationships, or even jeopardize their jobs.”
Institutional Stigma
Finally, as for institutional stigma, also called structural stigma, it’s essentially when the policies of private and governmental institutions restrict the opportunities for mental health support.
As the authors of this 2004 article explain, institutional stigma also includes major institutions' policies that may not be intended to discriminate but whose consequences nevertheless limit the options of people with mental health needs or disorders.
For example, a workplace may allow time off for an employee to attend physical therapy sessions, but not psychotherapy sessions.
Health insurance providers may offer a small copay to medical doctors and charge larger fees for visits to mental health professionals.
Or health insurance providers may offer a small copay to medical doctors and charge larger fees for visits to mental health professionals.
These types of discriminatory policies may have been justified due to ingrained societal or institutional beliefs that mental health isn’t as important as physical health or that mental health treatment is a luxury.
Thankfully, with the passage of the Affordable Care Act (ACA), everyone with coverage through a U.S. health insurance exchange marketplace plan now has access to mental health coverage benefits.

What are the effects of mental health stigma?
Over the course of a lifetime, as Mental Health America (MHA) points out, nearly half of all Americans will meet the criteria for a mental health disorder.
And, unfortunately, stigma has been found to be a major barrier in access to mental health care, as compared to physical health care.
Stigma has been found to be a major barrier in access to mental health care, as compared to physical health care.
According to Johns Hopkins Medicine, mental illness is now the leading cause of disability in the United States.
That said, the National Alliance on Mental Illness (NAMI) says only about 46 percent of those affected received treatment in 2020.
As Mordecai points out in his article for Kaiser Permanente, about 75 percent of American employees have struggled with an issue that affected their mental health. Yet, eight out of 10 workers with a mental health condition say shame and stigma prevent them from seeking mental health care.
A 2017 European study found that mental health patients who experienced self-stigma hindered their recovery, compared to those patients who did not experience self-stigma.
Mental health patients who experienced self-stigma hindered their recovery, compared to those patients who did not experience self-stigma.
According to the authors of this study, self-stigma often prevents us from seeking treatment for our mental health concerns because it can lead us to think negative thoughts about ourselves, and about the mental health condition(s) we may be experiencing.
When we think of ourselves as incompetent, or stupid—it can lead to feelings of low self-worth and depression—and worsening any mental health issues.
Additionally, thinking poorly of ourselves and our mental health condition can cause us to reject therapy and medications, consequently prolonging our suffering, and preventing improvement in our mood or symptoms.
Other consequences of mental health stigma include:
Discrimination in work, school or with housing
Bullying, physical violence or harassment
Substandard coverage for mental health treatment by health insurance providers
Low self-esteem, leading to hopelessness about our situation
Social isolation
What are the roots of stigma?
Fear is at the root of stigma.
Several studies show that stigma usually arises from lack of awareness, lack of education, lack of perception, and the nature and complications of the mental illness—for example odd behaviors and violence
As Julio Arboleda-Flórez, M.D., Ph.D., wrote in 2003, “the general public most frequently makes contact with mental illness through the media or the movies.”
After interviewing adults who had watched Joker, researchers concluded viewing the film was “associated with higher levels of prejudice toward those with mental illness."
A study published in April 2020 examined audience reactions to the 2019 movie Joker. In the film, the title character is a person with mental illness who becomes extremely violent.
After interviewing adults who had watched Joker, researchers concluded viewing the film was “associated with higher levels of prejudice toward those with mental illness."
Additionally, the study’s authors suggest that, for those audience members living with mental illnesses, watching Joker may increase their self-stigma, and consequently lead to “delays in help seeking."
Is mental health stigma reinforced by American media?
Mental health stigma is reinforced by cultural norms and messages we consume every day.
The media is a source of negative portrayals of people with mental illness and mental health issues.
Over the years, American TV news has frequently highlighted violent crimes committed by people with mental illness, which may have caused these types of crimes to appear more frequent to the viewing public.
In contrast, as this 2015 U.S. News and World Report article points out, studies reveal people with mental illness are less likely to commit crimes and are actually more likely to be victimized themselves.
“Do not describe an individual as mentally ill unless it is clearly pertinent to a story and the diagnosis is properly sourced,” the AP Stylebook instructs journalists and reporters.
To help address this, in 2013, the Associated Press (AP) Stylebook added an entry on mental illness to help journalists report on mental illnesses fairly and accurately. “Do not describe an individual as mentally ill unless it is clearly pertinent to a story and the diagnosis is properly sourced,” the AP Stylebook instructs journalists and reporters.
When including information about mental illness, the AP Stylebook tells journalists to identify the source for the diagnosis.
“Seek firsthand knowledge—ask how the source knows—and don’t rely on hearsay or speculate on a diagnosis,” the AP Stylebook says. “Specify the time frame for the diagnosis and ask about treatment. A person’s condition can change over time, so a diagnosis of mental illness might not apply anymore.”
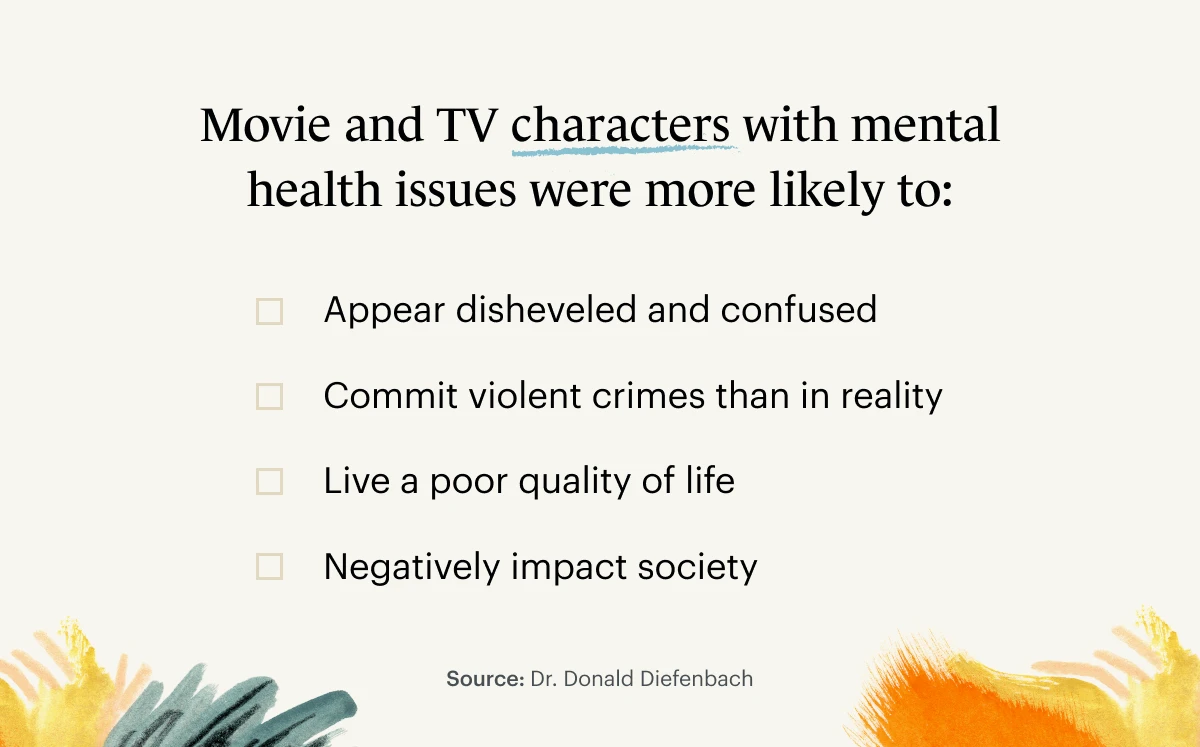
Movies and television shows also play a role in creating and promoting mental health stigma.
In an analysis of primetime TV characters with mental illness published in 1998, Donald Diefenbach, Ph.D., found that characters with mental disorders were found to be nearly ten times more violent than the general population of television characters, and 10-20 times more violent (during a two week sample) than all people with mental illness across the entire U.S. population over the course of an entire year.
These portrayals have a negative impact on people living with mental illnesses and conditions.
Movies and television shows also play a role in creating and promoting mental health stigma.
Negative media has a direct effect on a depressed person’s view of themselves. The reinforcement of self-stigma makes it harder for people to cope with their mental illness.
In a 2019 study of people with depression, participants experienced higher levels of self-stigma and lower mood after watching stigmatizing media of someone with depression.
These respondents also showed greater beliefs in stigma against depression, and an increase in self-stigma measures than respondents who watched neutral or non-stigmatizing media.
Thankfully, over the past twenty-five years, screenwriters have created some more nuanced and accurate depictions of individuals with mental health disorders in major movies and TV series.
Three examples of leading TV and film characters with mental disorders include the nuanced, thoughtful portrayals of:
Susanna Kaysen, an 18-year-old girl diagnosed with borderline personality disorder (BPD), played by Winona Ryder in Girl, Interrupted (1999)
John Nash, the Nobel Prize-winning economist with schizophrenia, played by actor Russell Crowe in A Beautiful Mind (2001)
Carrie Mathison, a CIA officer with bipolar disorder, played by actress Claire Danes on the Showtime original series Homeland (2011-2020)

How race, ethnicity, gender, and sexuality can contribute to mental health stigma
While media and national culture play a role in promoting mental health stigma, ethnic and racial minorities experience stigma differently.
Various cultural traditions, beliefs, and the role of minorities in society can contribute to a community’s experience of mental health stigma.
According to a 2020 article in BMC Public Health,“mental health stigma is higher among ethnic minorities than majorities.”
Asian-Americans and mental health stigma
Asian-Americans have often been described as “model minorities.”
This stereotype promotes a false and dangerous idea of perfectionism.
Pressure to live up to such a label can cause shame when problems and mental health challenges arise for Asian Americans.
Asian Americans are less than half as likely as Caucasians to use mental health services.
In fact, it’s this shame and self-stigma that often prevents Asian Americans from seeking mental health treatment.
In fact, Asian Americans are less than half as likely as White Americans to use mental health services. Find out more about why that may be in this article.
“For some Asian Americans, there’s a real sense that your value as a person depends on your ability to take care of your family and community,” Dr. Geoffrey Liu, M.D., a psychiatrist at McLean Hospital explains why Asian Americans don’t seek mental health help.
“This way of thinking originated, for East Asians, from an ancient philosophical tradition called Confucianism," Liu says. "Mental illness is seen—and I should emphasize, incorrectly—as taking away a person’s ability to care for others. For that reason, it’s seen as taking away someone’s identity or purpose. It’s the ultimate form of shame.”
Black Americans and stigmas around mental health
Even with Black celebrities such as Jay-Z, Kerry Washington, Michelle Obama, and Gabrielle Union speaking openly about their positive experiences with therapy and counseling, today there are still many stigmas around mental health and therapy among African Americans.
Among Black Americans, the experience and prevalence of community can contribute to public mental illness stigma.
In Black communities, churches and faith-based organizations can play a stronger role in counseling and care when individuals experience mental health crises.
A mental health crisis can be perceived as counter to the community.
For Black Americans who have historically valued family, church, and community highly to survive, there can be a significant stigma against pursuing any individual-focused activity that may be perceived as focusing negative public opinion aimed at the group as a whole.
As MHA points out, despite progress made over the years, racism continues to have an impact on the mental health of Black Americans.
What’s more, historical and contemporary instances of exploitation and negative treatment have led to a distrust of authorities, many of whom are not seen as having the best interests of African Americans in mind.
Mental illness is also perceived as a weakness by African Americans.
This perception is especially true for African American women. Historically, Black women have had to endure many hardships in America, but have survived. That historical strength created the myth of the “strong Black woman,” essentially someone who is able to withstand adversity without crumbling under pressure.
This stereotype inadvertently exacerbates the stigma around Black women seeking therapy and mental health support. Consequently, self-stigma and public stigma may prevent African American women from seeking therapy when they need it.
Mental health stigmas in Hispanic and Latinx cultures
As with Asian-American and African-American communities, cultures within the Hispanic and Latinx community place a strong value on family, community, and collectivism.
In this social framework, caring for mental health is considered an individual exercise, and therefore deprioritized.
Machismo is the belief that men should be strong, stoic, and protectors of the family. Marianismo is the belief that women should be moral, self-sacrificing and suffer in silence.
The concepts of machismo and marianismo contribute to mental health stigma in Hispanic and Latino cultures.
Machismo is the belief that men should be strong, stoic, and protectors of the family. Machismo is the belief that women should be moral, self-sacrificing and suffer in silence.
Having a mental illness, and pursuing treatment, go against both gender concepts. A man with a mental illness is thought of as weak and unable to provide, whereas a woman with a mental illness is also seen as weak, and unable to fulfill her support role in the family.
LGBTQIA+ community mental health stigmas
The stigma, prejudice, and discrimination members of the LGBTQIA+ community face can lead to unhealthy coping tactics create barriers to mental health care.
The National LGBTQIA+ Health Education Center found members of the LGBTQIA+ community are:
Less likely to have health insurance
More likely to experience discrimination from medical and health care staff
More likely to discover that clinicians do not have knowledge in caring for them
According to the 2015 U.S. Transgender Survey, in the previous year “33 percent of transgender people had at least one negative experience with a health care provider, such as being refused treatment because of gender identity.”
American men’s stigma around getting mental health support
Across many cultures and societies, including modern-day America, men are often encouraged or even expected to be tougher and to hide their emotions.
40% of American men were told as children that: "men don't complain about health issues."
This expectation and the resulting stigma around men seeking therapy or men discussing their mental health struggles contribute toward less American men than women seeking counseling and therapy and mental health support.
According to a 2019 Cleveland Clinic survey of over 1,000 U.S. males, 40 percent of American men were told as children that: "men don't complain about health issues."
The same survey found that only 50 percent of American men engage in preventative care by seeing medical doctors for routine check-ups.
And it also found that 72 percent of men "would rather do household chores, like cleaning the bathroom or mowing the lawn, than go to the doctor."
This brand of masculinity is presented to children early in life and reinforced by most of the media they consume.
Pressure to conform to this macho mold comes from all sides.
Failure to embrace traditional masculine gender roles can result in exclusion, bullying, and lack of social opportunity.

Steps we can all take to reduce and even completely end stigma
Stopping mental health stigma involves tackling the problem at each level: self, public, and institutional.
3 ways to combat stigma, according to McLean Hospital:
Educate yourself and others about mental illness
Protest against unfair depictions of mental illness
Interact with people who experience mental illness
Social media platforms, such as Instagram, Facebook, TikTok, and Twitter, can play an important role in both spreading and smashing the stigmas around mental illness.
2019 research on Twitter messages found that mental health conditions were subject to more stigmatizing and trivializing attitudes than physical health.
The more you know the truth about real people living with mental disorders, the less likely you will be to buy into stereotypes.
One of the most effective ways to reduce stigma is connecting with others who have mental illnesses. You can do this by joining online communities, by following certain hashtags, and in real life by volunteering with local groups.
The more you know the truth about real people living with mental disorders, the less likely you will be to buy into stereotypes.
To end self-stigma, the National Alliance on Mental Illness (NAMI) suggests talking openly about your mental health, including your treatment approach.
Being open will help reduce any shame you may feel about your experiences. And the more you discuss your mental health, the easier it becomes for you and others to be honest.
NAMI also suggests becoming productive in other areas of your life.
Accomplishing goals and tasks will help improve your self-esteem, and give others a more accurate representation of what living with a mental health condition is like.
Being open will help reduce any shame you may feel about your experiences. And the more you discuss your mental health, the easier it becomes for you and others to be honest.
Also, individuals with mental illness can help reduce public and institutional stigmas by reaching out to companies, groups, and the media.
Speak up when mental illness is portrayed incorrectly in the media.
And write to lawmakers and companies about mental health policies to make changes.
Openness, authenticity, education, and activism are the most powerful ways to combat mental health stigma at all levels.
These steps call attention to the issue and should result in more people being treated with care and dignity.
Finally, discussing mental health on a regular basis with friends and family will begin to lessen the taboos around these topics and aid in stopping the stigmas around mental health so we can—eventually—completely put an end to stigma.

READ NEXT: How and Why Talk Therapy Actually Helps
Need to find a therapist near you? Check out the Monarch Directory by SimplePractice to find licensed mental health therapists with availability and online booking.





