Historically, movies and TV shows have always made it seem like people with OCD, also known as obsessive compulsive disorder, present symptoms in a very specific way.
Many characters are portrayed doing things like excessive hand washing or turning light switches on and off a particular amount of times.
In fact the lack of diverse and accurate portrayal of people with OCD (obsessive compulsive disorder) in the media can cause the public to misunderstand the disorder.
Even individuals who have obsessive compulsive disorder may not be aware of the various OCD symptoms.
So it’s no wonder why many people tend to misunderstand this disorder.
Below we dig into the statistics, facts and details around what is OCD, what are the treatments for OCD, and how OCD is diagnosed.
First, what is OCD and what are the main OCD symptoms?
The American Psychiatric Association (APA) cites that obsessive compulsive disorder (OCD) is a disorder in which people have recurring, unwanted thoughts, ideas or sensations that make them feel driven to do something repetitively.
And according to the International OCD Foundation, there are two hallmark symptoms of OCD—obsessions and compulsions.
When a person has obsessive compulsive disorder they will get trapped in a constant cycle of these two symptoms—first an obsession, and then a compulsion—as they try to find a way to navigate their feelings of distress.
So what are obsessions and compulsions when it comes to OCD?
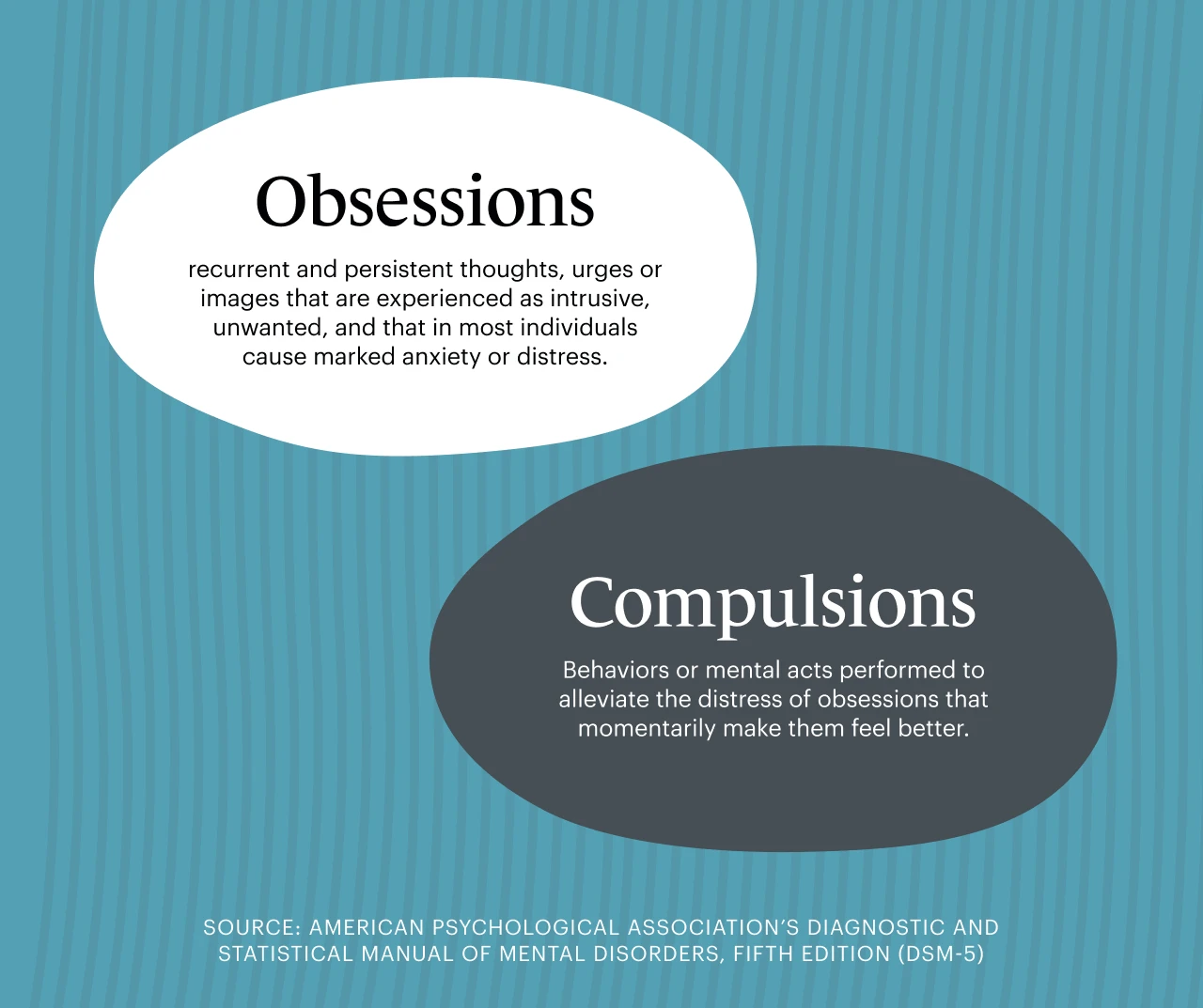
The American Psychological Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines obsessions as “recurrent and persistent thoughts, urges or images that are experienced, at some time during the disturbance, as intrusive, unwanted, and that in most individuals cause marked anxiety or distress.”
This means that in order for a person to alleviate this level of obsessive distress, they need to find behaviors, or compulsions—that momentarily make them feel better.
Until they don’t.
Often times the obsessive thoughts or urges return more powerfully than before and the compulsions are repeated to a point that it begins to actively interfere with a healthy way of life.
People with OCD spend at least one hour a day dealing with obsessions and compulsions, according to the National Institute of Mental Health (NIMH).
And, in fact, many OCD sufferers spend much more time dealing with symptoms.
According to the APA’s DSM-5, one to three hours is considered mild to moderate OCD, while in those with severe OCD, the obsessions and compulsions are so constant that they are disabling to the individuals experiencing them.
Let’s take a closer look at what obsessions and compulsions can look like when questioning what OCD is.
Obsessions
The key thing to remember when it comes to obsessions is that they are unwanted.
For example, the more a person tries to control them, the further they spin out of control, intensifying the feelings of anxiety and fear.
While many people experience intrusive thoughts at some point, they tend to brush the thoughts away and not assign them any importance.
For someone with OCD, however, the thoughts are ominous. They seem to say something scary about who you are. They are a monster standing in your way, casting a shadow over your entire life.
5 OCD obsessions
While most people are familiar with the type of OCD that causes a person to compulsively clean, the other themes may come as a surprise.
Here are the 5 primary OCD obsessions, according to MedlinePlus:
Requiring a symmetrical, organized environment
Fear of contamination from germs or dirt
Intrusive, horrifying, and traumatic thoughts of harming loved ones or yourself
Unwanted images of violent, religious, or sexual acts
Fear of losing something
You may have OCD and not even know it if:
You have a deep fear of stabbing a family member and no amount of self-reassurance seems to make it go away
You find yourself repeatedly turning around to check whether you left the stove on, making you continually late for work
An unwanted image of you committing an act of sexual violence plagues your mind and won’t leave you alone

Compulsions
It’s no wonder this disorder can be debilitating. And that’s precisely why people with OCD perform compulsions: they want to feel better.
6 OCD compulsions
Compulsions can look like straightening boxes of pasta to make sure they all face the same way—something you’d probably see in a TV portrayal of OCD.
Or, they can look like repeating a thought or phrase to assure yourself that you would never act on a violent intrusive thought.
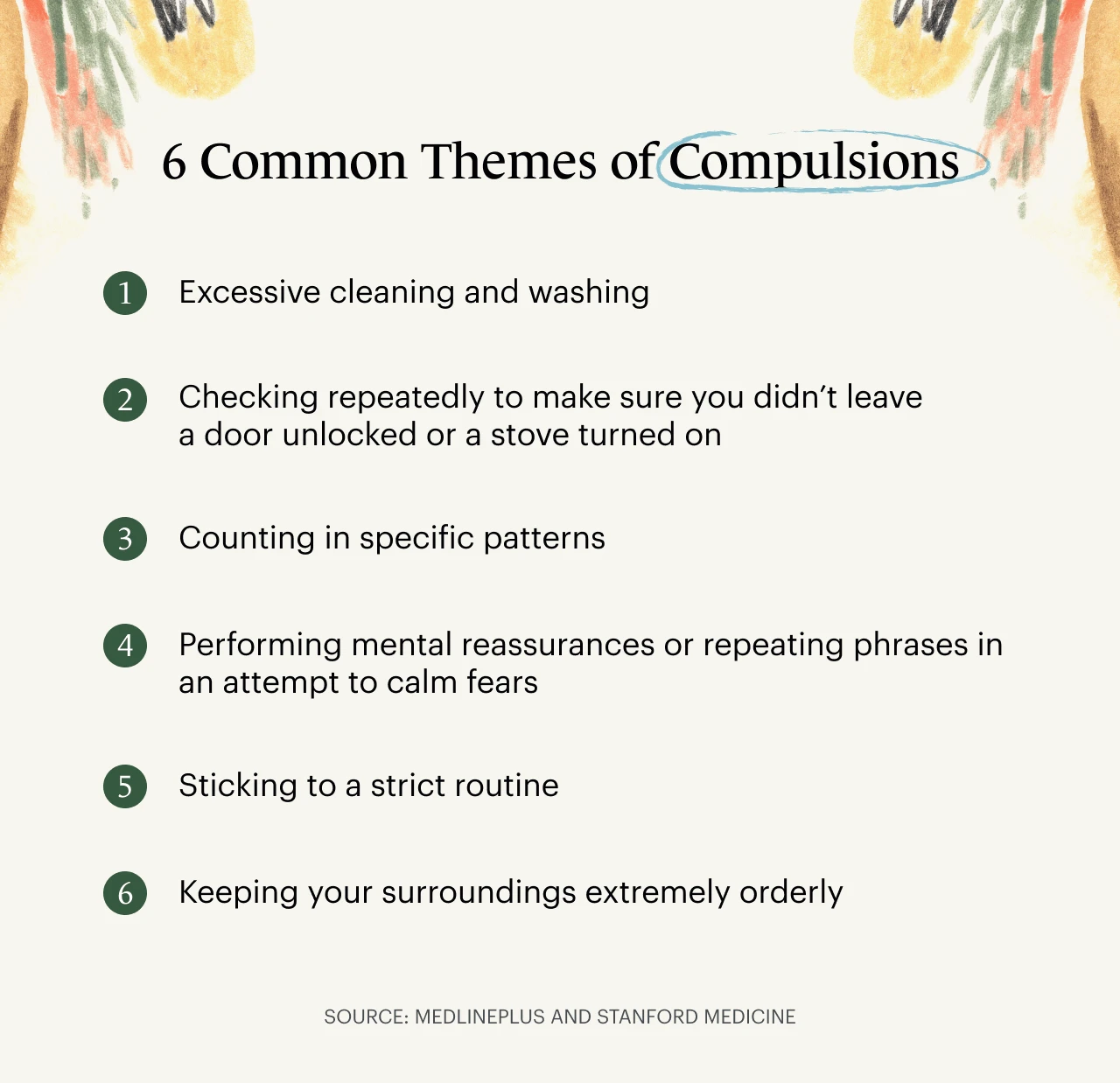
According to Stanford Medicine some of the common themes for compulsions are:
Excessive cleaning and washing
Checking repeatedly to make sure you didn’t leave a door unlocked or a stove turned on
Counting in specific patterns
Performing mental reassurances or repeating phrases in an attempt to calm fears
Sticking to a strict routine
Keeping your surroundings extremely orderly
What percentage of Americans have OCD?
The National Comorbidity Survey Replication (NCS-R) found that between 2001 and 2003, 2% of American adults had OCD either currently or at some point in their lives (lifetime prevalence). Of these, 1.8% were female and 0.5% were male. This data was collected roughly 20 years ago and did not include youth.
The DSM-5 states that 1.2% of adults in the United States live with OCD during any given set of 12 months, a measurement referred to as twelve-month prevalence.
Since OCD is usually a lifelong disorder that can develop at any time, including during childhood, the true impact of OCD may be higher than these numbers can convey.
The International OCD Foundation estimates that two to three million adults in the United States—about one in 100—live with OCD. Picture the entire city of Chicago having OCD!
Additionally, the International OCD Foundation believes that in the United States, about one in 200 children, or about 500,000 youth, live with OCD.
How has the definition of OCD changed in the APA's DSM-5?
When the DSM-5 came out in May of 2013, it brought significant changes to the definition of OCD.
The biggest change was that OCD moved out of the Anxiety Disorders class and into a new class: Obsessive-Compulsive and Related Disorders.
In addition to OCD, this new class includes skin-picking (excoriation) disorder, hoarding disorder, hair-pulling disorder (trichotillomania), and body dysmorphic disorder.
While OCD undoubtedly causes anxiety—and many people with OCD also have an anxiety disorder—OCD is thought to impact the brain differently, causing repetitive behaviors rather than the avoidant ones that define anxiety disorders.

In the past, researchers believed that people with OCD did compulsions to ease the anxiety brought on by obsessions.
A newer understanding of OCD as reflected in the DSM-5's creation of a new class, is that a compulsion is more of a rigid, automatic thought or behavior that hijacks the brain’s problem-solving capacities.
As the DSM-5 still defines compulsions as mental acts or repetitive behaviors aimed at easing the anxiety an obsession brings, the answer to whether OCD is an anxiety disorder or a repetition disorder may lie somewhere in between these two theories.
In addition to this major change, some of the criteria for diagnosing OCD were dropped or expanded on in the DSM-5.
You can see a side-by-side comparison of the changes here.
What are the different types of OCD?
The DSM-5 doesn’t define official subtypes of OCD, but it does outline some of the most common “symptom dimensions,” including obsessions and compulsions related to cleaning, symmetry, taboo thoughts, and fears of harming others.
These are reflected in some of the OCD subtypes put forth by the International OCD Foundation and the OCD Center of Los Angeles:
Contamination obsessions: worrying that germs, substances, and other unpleasant things or ideas have contaminated you and you must decontaminate yourself
Harm OCD: intrusive, traumatic thoughts or images of harming yourself or others
Perinatal OCD: OCD that kicks in during or after pregnancy and revolves around constant fears about causing harm to the baby
Sexual Obsessions: Unwanted thoughts or mental images related to sex, including: fear of acting on a sex-related impulse, fears about sexually harming children, relatives, or others, and fears about aggressive sexual behaviors towards others
Relationship OCD (ROCD): questioning whether you’ve found “the one” and constantly checking to see if you’re making the right decision about your relationship
Sexual Orientation OCD: obsessive fears and doubts about being heterosexual for LGBTQIA2S+ folks, and vice versa for heterosexual people
Religious/moral obsessions: constantly worrying you have broken the laws or ethical code of your religion or faith system
Some people may struggle with more than one of these subtypes. In others, none of these subtypes ring true—and that’s because this isn’t an exhaustive list.
There are numerous variations of OCD, which you can learn more about in this guide to OCD types from the recovery-based charity, OCD-UK.
What triggers OCD?
There isn't one single, known cause for OCD, but it's believed that genetics, brain chemistry, and a person’s environment may all play a role. In all these areas, research is still underway, and providers and researchers are still learning new information that may help improve OCD diagnosis and treatment.
Some family studies have found that people with close relatives, like a child, parent, or sibling, who have OCD are at a higher risk of OCD themselves.
In addition to genetic connection, brain chemistry and structure can have an impact on whether or not someone has OCD.
Some brain imaging has shown that there seems to be a connection between OCD symptoms and differences in the structure of the frontal cortex and subcortical structures in the brain.
Lastly, a person’s environment may have an impact on an OCD diagnosis. In some studies, an association between childhood trauma and OCD symptoms have been reported—but more research is needed to understand this relationship better.
Although the reasons for the disorder appear to be diverse and some causes still elude us, a 1990s case-controlled study of children ages 4-13 found that children who had been recently diagnosed with OCD, Tourette’s Syndrome, or tic disorder were more likely than the control group of children to have had a prior streptococcal infection.
The study’s authors concluded that in some cases, OCD may arise as a result of a postinfectious autoimmune phenomenon induced by childhood streptococcal infection.
How to get diagnosed with OCD?
The first step toward getting an OCD diagnosis is finding a therapist who specializes in treating OCD.
Your therapist will ask you about your symptoms and assess how they match up to the diagnostic criteria in the DSM-5.
To obtain a diagnosis, you must:
Have obsessions or compulsions, or both
Suffer from internal distress or avoidance of certain situations, such as social gatherings, as a result of obsessions and/or compulsions
Experience these thoughts and behaviors for at least one hour a day
Not be taking medications or drugs that could cause obsessions and/or compulsions
Not have another explanation for the symptoms, such as general anxiety disorder (GAD) or an eating disorder
Of course, it’s possible to have both GAD and OCD, or GAD, OCD, and an eating disorder. A skilled OCD therapist can use other diagnostic tools to evaluate whether you have any concurrent diagnoses along with OCD.

Does OCD go away?
For most people who live with it, OCD is an unpreventable, lifelong condition—but there’s still plenty of hope.
If you believe you have mild or moderate OCD, it’s important to seek out treatment as soon as you can. Early diagnosis and treatment may help keep OCD from getting worse.
If you are already spending hours every day trying to control relentless obsessions and compulsions, please know that help is available. You don’t have to keep suffering in silence.
Treatment for OCD
According to the ADAA,Cognitive-behavioral therapy (CBT), medication, and exposure and response prevention (EX/RP) can all help treat OCD.
In addition to the options above, mindfulness, which is the practice of staying present and allowing thoughts to course through the mind without judgment, can also be an important component of treating OCD.
According to Jon Hershfield, MFT, and Tom Corboy, MFT, in their book, The Mindfulness Workbook for OCD: A Guide to Overcoming Obsessions and Compulsions Using Mindfulness and Cognitive Behavioral Therapy: “The practice of mindfulness for OCD is a cultivation of a relationship between you and your mind in which you cooperate with one another in the development of mastery of the disorder.”
As you work with your therapist, they may recommend one of these strategies or a combination of all of them to help you to figure out what type of treatment delivers the most impact and success.
How to find mental health support for OCD
If you are struggling with OCD symptoms, you may feel hesitant to reach out for help.
Finding a therapist who specializes in treating clients with OCD can help you find ways to manage your symptoms and live a happy and balanced life.
The Monarch Directory from SimplePractice makes it easy for you to find a therapist in your area with experience treating OCD.
Symptoms of OCD can be terrifying, but you’re not alone. Help is just a quick search away.
READ NEXT: Only One Form of Therapy Helped Me Control My OCD
Need to find mental health professionals who specialize in clients with OCD near you? Check out the Monarch Directory by SimplePractice to find therapist and counselors who specialize in OCD and other disorders with availability and online booking.
About OCD: What is OCD? Retrieved from the International OCD Foundation website: https://iocdf.org/about-ocd/
Obsessive-Compulsive Disorder. (2021, February 23). Retrieved from MedlinePlus website: https://medlineplus.gov/obsessivecompulsivedisorder.html
Obsessive-Compulsive and Related Disorders. Retrieved from Stanford Medicine website: https://med.stanford.edu/ocd/about/symptoms.html
Obsessive-Compulsive Disorder. (2019, October). Retrieved from National Institute of Mental Health website: https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd
Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health [Internet]. Retrieved from the National Library of Medicine website: https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t13/
Obsessive-Compulsive Disorder (OCD). Retrieved from the National Institute of Mental Health website: https://www.nimh.nih.gov/health/statistics/obsessive-compulsive-disorder-ocd
Who Gets OCD? Retrieved from the International OCD Foundation website: https://iocdf.org/about-ocd/who-gets/ OCD Center of Los Angeles – Treatment for OCD and Related Conditions. Retrieved from OCDLA website: https://ocdla.com
Subtypes of OCD. Retrieved from the International OCD Foundation website: https://iocdf.org/expert-opinions/subtypes-of-ocd/




